Why Do We Segregate Older Adults?
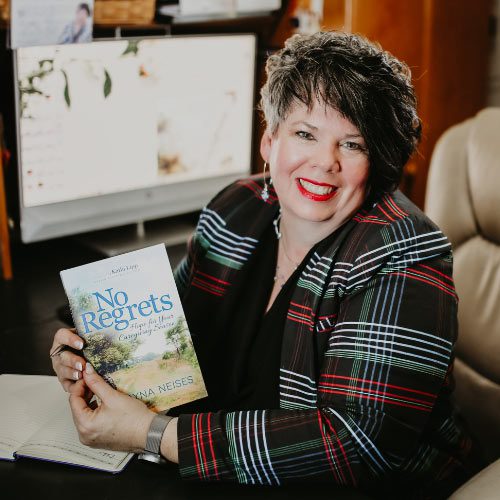
Dr. Mary L. Flett is a licensed psychologist with more than 20 years experience working with behavioral health issues in older adults. She specializes in assessment and treatment of dementia, chronic pain, and emotional and spiritual issues associated with Aging. A Buddhist, Dr. Flett uses mindfulness to work with mind/body/spirit approaches for optimal wellness. Her warm and engaging writings offer unique insights about what it means to create purpose and meaning across the lifespan. You can read more from Dr. Flett at her new website, www.FivePillarsofAging.com. Her books, which focus on successful aging, can be found on Amazon.
This is the first part of our interview. It has been edited for length and Clarity.

Ben: Can you tell us a bit about your background and how it led you to having a career in aging?
Dr. Flett: The reason why I have spent my entire professional career working with aging adults is because my maternal grandfather became wheelchair-bound when I was very young. And this was back in the 1960s, before we had modern-day Medicare, and the cultural norm was for families to care for parents. And my grandfather was a widower.
We lived in a nearby community. I grew up in the suburbs of Chicago; my grandfather lived in Oak Park and we lived in River Forest, which was just about next door to one another. Every day, either my mother or I would go over and make sure that he was okay and that he had food and that his needs were met and didn’t then think twice about that. And Friday nights, I would go over and have chicken pot pie and chocolate ice cream and stay overnight and make breakfast for him. For me, it was just an extraordinarily precious and wonderful time with a man whom I adored, who shared wonderful stories. My grandfather was an electrical engineer. He grew up in Wisconsin before the turn of the last century and had done very well for himself. He went to college, which was unusual. He married a woman who also went to college, so I had grandparents who were college-educated. University of Wisconsin, Let’s go Badgers!
The expectation in our family was always to care for one another, respect one another. Be curious about life. Read as much as you absolutely can. Take advantage of every opportunity to grow and learn and expose yourself to new and wonderful things. And I thought everybody lived like that. Now, flash forward a few years. I went to grad school for psychology, when I was in my late 30s, so I had a couple of other careers before then. I was studying psychology and realized that I really liked working with people who were mature and who had some life experience. And even though maybe they were challenged by those life experiences, they still came from a sense of rootedness and were willing to work on their challenges. And as you well know, there are many challenges: physical challenges, social challenges, Grief, and loss. And these were all things that I had developed some pretty good skill sets with. It just made sense for me to continue to work with aging adults. And oh yeah, by the way, I became an aging adult, so it was sort of like rehearsal for me and I got taught an awful lot. I hope I did some good for them, but I was pretty much on the receiving end of things.
Ben: What do you think are some of the most prevalent challenges emotionally that adults face as they get older?
Dr. Flett: I think the biggest two problems compete against each other. One is isolation and loneliness. Our culture does not value — nor does it have any way of actively integrating — elders – unlike generations before. And unfortunately, we see literal segregation of people 55 and older into communities like Del Webb or The Villages, all of which are portrayed as wonderful places to grow old with your peers. The problem is that growing old with your peers turns out not to be all that beneficial. And having younger people involved is really very healthy. The second problem, emotionally, is a change in status, transitioning from “doing” to “being.” Our culture highly values productivity and the very nature of aging is for us to become less productive. But it also turns out there are fewer opportunities for being productive. While someone might have great ideas and be entrepreneurial throughout their lifespan, they may not have the opportunity to use those skills or try out new things. Because again, we are segmenting the older population. And we do it, interestingly enough, purely chronologically as opposed to functionally or through a capacity. I know many people who may have challenges around mobility or challenges using their hands because of arthritis, or perhaps they have a chronic condition like Parkinson’s, but they’re still vital and engaged and could be contributing to enormous amounts of things. But because we’ve identified them as being a certain age and having certain functional limitations, we no longer value them. We put a label of “handicapped” or “disabled” on them, which I think does them a disservice and cuts us off from enormous amounts of resources that could be beneficial and help us.
Ben: That’s really interesting. And scary to think about how we’re so accepting of aging this way. For sake of definition, who do you consider to be an older adult?
Dr. Flett: Technically speaking, there are four different definitions of old and we start with the young old. And that basically is anyone 55 to about 65 or 70. Then we have the old, who are about 70 to 79. Then we have the older old, who are the 79 to 90-year-olds. And now there’s a fourth category of the oldest old, who are 90 to 100 and above. Obviously, the language is awkward at best.
I much prefer to look at aging as both a developmental and a functional way of measuring a person’s ability to be in the world. The developmental has to do with the body breaking down, the physiologic. So, we start to see the brain actually breaking down at about age 30. We see some physical breakdown of organs and things like that, depending on what you’re exposed to and what you undergo in terms of Stress and put in your body, around 45-50. If you are using all your skills cognitively and you are healthy and you’re eating well and doing all else you can to care for yourself, you’re still going to see, around 60 to 65, decrease in capacity and muscle strength, and you may see a decline in your teeth and a variety of other things. My grandfather remained incredibly cognitively intact, even though he had a Stroke, until he was 82. I unfortunately have a dear friend in her 80s whose son is in his 50s and he’s just recently been diagnosed with a very severe form of dementia called frontal lobe dementia. Though he’s in his 50s, he’s not able to care for himself anymore, which is the criterion we typically use to identify a dependent. It works more easily for insurance purposes and the government to use a number, but that is inaccurate from truly a societal perspective.
Now, I’ve seen some recent research that shows if you don’t act your age, you won’t feel your age in the simplest sense. The most unscientific way to explain this is that if you’re hanging out with people younger than you or doing things younger than a typical person your age, whatever their activities are, that might impact both your physical health as well as your mental and emotional health.
Ben: I’m just thinking about places like The Villages, which have grown in popularity over the last several years. I think a lot of people are shocked just at how many people actually live there. I’ve read about some cutting-edge medical work going on there around aging. But they’re still doing it in a very segregated way. And I know that’s a very different sort of situation than moving into something like memory care if you develop dementia and you need that level of care. I can see a lot of benefits to living in a place like The Villages. But according to this assessment, it might not be the best decision to leave multigenerational neighborhoods.
Dr. Flett: There’s a couple of ways of answering that. The benefits of an intergenerational relationship, and I’ll speak just from my own personal experience, having my grandfather mentor me, love me, father me. It was absolutely invaluable to my life. And I know many other people who talk about the benefits of having an older adult and older caregiver provide them with these things. I have friends for whom that was the only way they could afford to live, with support from a grandparent. So they had multi-generations in the house. But there are stressors inherent with that. There’s privilege inherent with being able to access Wisdom, but not everybody who is old is wise. So the challenge here, I think, is really in redefining what it means to be a member of a community. And in particular, what an elder-friendly community might look like.
Let me speak directly to what we were talking about here. Del Webb was the first guy to ever develop a special place for older adults. He did it in the 1960s. The man was a real-Estate developer. And he wasn’t thinking about older adults and all their special needs and all the rest of that. He saw an opportunity to sell a bunch of homes to a post-war generation that didn’t have anything to do. There was still an expectation based on hard numbers — actuarial numbers — that people would only live to about 68, 69. Living to 75 was really outside the range of expected lifespan.
When you think from a real-estate development perspective, you’ve got a whole group, a whole generation of people coming in who will buy a home, pay it off, sell it and then have another group right behind them coming in. It’s brilliant. That’s good Money. What has happened is that the Boomer Generation has defied a lot of these actuarial expectations. The idea that this happened with Nursing homes is similar. The idea that you would move into a nursing home, occupy a bed for maybe three to five years, has been blown out of the water.
People are now moving into developments like Del Webb Homes which were built in the 60s. The homes now need an enormous amount of refurbishing and remodeling to meet the needs of a population that’s changing. I talk about this in terms of adaptation and accommodation. We have where you live. That’s part of a community you choose to live with, which is an incredibly important part of community definition. Then there are all of the adjunct services that are necessary to meet the needs of that community. And when we look at it more from that dimensional aspect, you start to see it’s not just a home that you could buy for a reasonable amount of money with not much upkeep and a neighbor who’s your same age at a golf course and a pool. Now we start to see the need for churches and other spiritual connections. You start to see the need for Exercise and physical Therapy. We start to see the need for medical services delivered in a variety of different ways. We start to see the need for long-term care for memory care. None of these things were contemplated initially.
But if you look overseas, especially in England and Australia and New Zealand right now, there are a lot of very creative ideas around creating elder-friendly communities where people age in place. And the places themselves include not just the home, but all of the adjunct services that are required: all the plug-ins, all the peripherals, if you will, are designed to be adaptive and accommodating. So the adaptations that are needed are going to be for people who have cognitive problems or physical problems. An easy transportation system, that’s an adaptation. The accommodations can be at the individual level, and your company [Joe and Bella] is so perfect about this because you’re creating clothing that can accommodate various functional needs as well as the cognitive needs of people. So to have that flexibility, to have that vision, has never before been needed in such numbers as it is today around the world, because the Baby Boomer generation is the first to be stretching these boundaries of age, which turns out to pull enormously and tax enormously our cognitive capacities.
We don’t really know what dementia is. We know that there are fundamental changes in the brain. If we only understood the brain more than we do now, we could maybe predict what these fundamental changes are going to be. But we understand that the level and care needed by people who have functional cognitive impairment grows each year. And then towards the end of their life, the demands are for full care, even though cognitively they’re no longer available.