Too Many Ills! Too Many Pills!
Photo by Myriam Zilles on Unsplash
This week I learned a new word – “polypharmacy.” I also learned that I could be a poster child for it.
Doctors define polypharmacy as the regular use of five or more medications. It is a common situation among us chronologically gifted folk because many of us take medicines for two or more chronic conditions.
This isn’t necessarily a problem, but it can be. Multiple medications are absolutely necessary for some conditions, but the greater the number of medicines we ingest, the higher the safety risks.
When multiple medicines cause a patient more harm than good, polypharmacy becomes “medication overload.” The Lown Institute, a nonpartisan think tank, argues in Its 2019 report, Medication Overload: America’s Other Drug Problem, that Americans are experiencing an epidemic of medication that is particularly harmful to older adults. According to the report, more than 40% of older adults take five or more prescription medicines daily, and 20% take ten drugs or more.
But before I lob any metaphorical firebombs at the medical-pharmaceutical-industrial complex, I feel obliged to be fully transparent about my own regimen, which illustrates the problem. Here is the complete catalog of my daily meds:
Prescription:
4 pills for Depression/mood disorder
1 pill for cholesterol
1 pill for hypertension
1 inhalation for asthma
Non-prescription:
2 pills for multivitamins
2 pills for calcium/Vitamin D
1 pill for nasal congestion
1 inhalation for allergies
Depositing 7 prescriptions and 13 total drugs daily into my body certainly qualifies as polypharmacy, but is it medication overload? Keep reading, then you decide.
The Safety Issue
The safety problem is that each additional medication increases the risk of suffering a serious, possibly life-threatening side effect. We’re not talking nausea or dry mouth; we’re talking delirium, impaired cognition, internal bleeding (including bleeds in the brain), and falling.
Medicines are chemical compounds, and some chemicals just do not play well with others. Many harmful drug interactions are well documented, and alert physicians and pharmacists know to avoid them. Yet in spite of that, over one recent decade, serious adverse drug events sent older adults to emergency rooms or other treatment 35 million times, according to the report. People over 65 suffer disproportionately – at only 14 percent of the population, older adults account for 56% of hospitalizations for adverse drug events.
The Lown Institute report offers some credible explanations for why this happens.
Fragmented Health System
If you only see one doctor for all your health needs, you should not have medication risk. (And if you do, you know who to blame.) But that’s highly unusual. More likely, you see specialists for specific conditions. Each specialist treats your particular condition separately, often without knowing your full medical history, other conditions you have, or other medications you’re taking. The older we get, the more likely we are to have multiple chronic conditions and multiple doctors. (Even mixing in over-the-counter meds with prescriptions can wreak havoc.)
The risks multiply whenever a patient transitions from a hospital to a rehab center or Nursing home. Drugs that were prescribed during the hospital stay for short-term, acute conditions may be continued long after they are appropriate. A full medical history may not be understood by the (understaffed and overworked) personnel of a long-term facility. The patient has no advocate in coordinating the medications of multiple specialists. As a result, patients frequently end up taking more medicine than necessary, and running more risks of adverse drug reactions.
Prescription Culture
We live in a society convinced that there is “a pill for every ill.” Aging is treated not as a natural process but as a disease, and death is the failure to cure it. We are also a society exceedingly fond of instant results. Resolving a problem by taking a pill is easier and faster than making long-term Lifestyle changes.
These tendencies have been exacerbated by decades of pharmaceutical advertisements that imply a cause-effect relationship between taking prescription drugs and blissful, pain-free living. The industry spends more than $20 billion annually marketing to the medical community, and another $6 billion advertising directly to consumers. (The U.S. is one of only two countries that permit the latter.)
Information Gaps
After several decades of working out the kinks, electronic medical records have achieved their primary purpose: efficient billing. Recording and sharing clinical information on patients, however, is often less than smooth. Patient confidentiality is one of many obstacles to allowing access to all medical personnel.
There are also gaps in what is known about medication overload, and particularly for older patients. One reason: Older adults are rarely invited to participate in clinical trials for new drugs.
Age Matters
All other reasons aside, there is another reason medication overload impacts older adults disproportionately. It is normal as we age for lungs, kidneys, and liver to work less efficiently. In short, our metabolism slows, and it takes longer for a dose of medicine to work its way through our system. What was a safe dose for years may increase the risk of adverse drug reactions as our bodies age.
The Lown Institute report argues that physicians must do more deprescribing – reducing the load of medications in patients by stopping medicines that are no longer necessary, or were never necessary, or were not beneficial. Also, the report notes, deprescribing needs more attention in medical and pharmacy Education.
The John A. Hartford Foundation and the Institute for Healthcare Improvement are also attacking the medication overload issue through their joint Age-Friendly Health Systems initiative.
My Bottom Line
In spite of taking 13 prescription and over-the-counter drugs every day, I consider myself pretty healthy. I am lucky that my two prescribing doctors are both in the same medical system and have full access to my electronic records. Both are good about taking a big picture view of my health. I haven’t had any adverse drug reactions – yet.
But if that changes as my internal systems continue to rust, I will be prepared.
Has Your Transition Been Bumpy? Let’s Talk About It
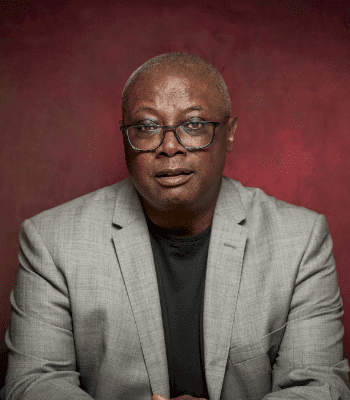
I want to interview people about their own Retirement experience for a book I’m researching. If you care to share your story, please email me at don@donakchin.com to set up a remote interview.