The Health Care System Is Failing Older Americans
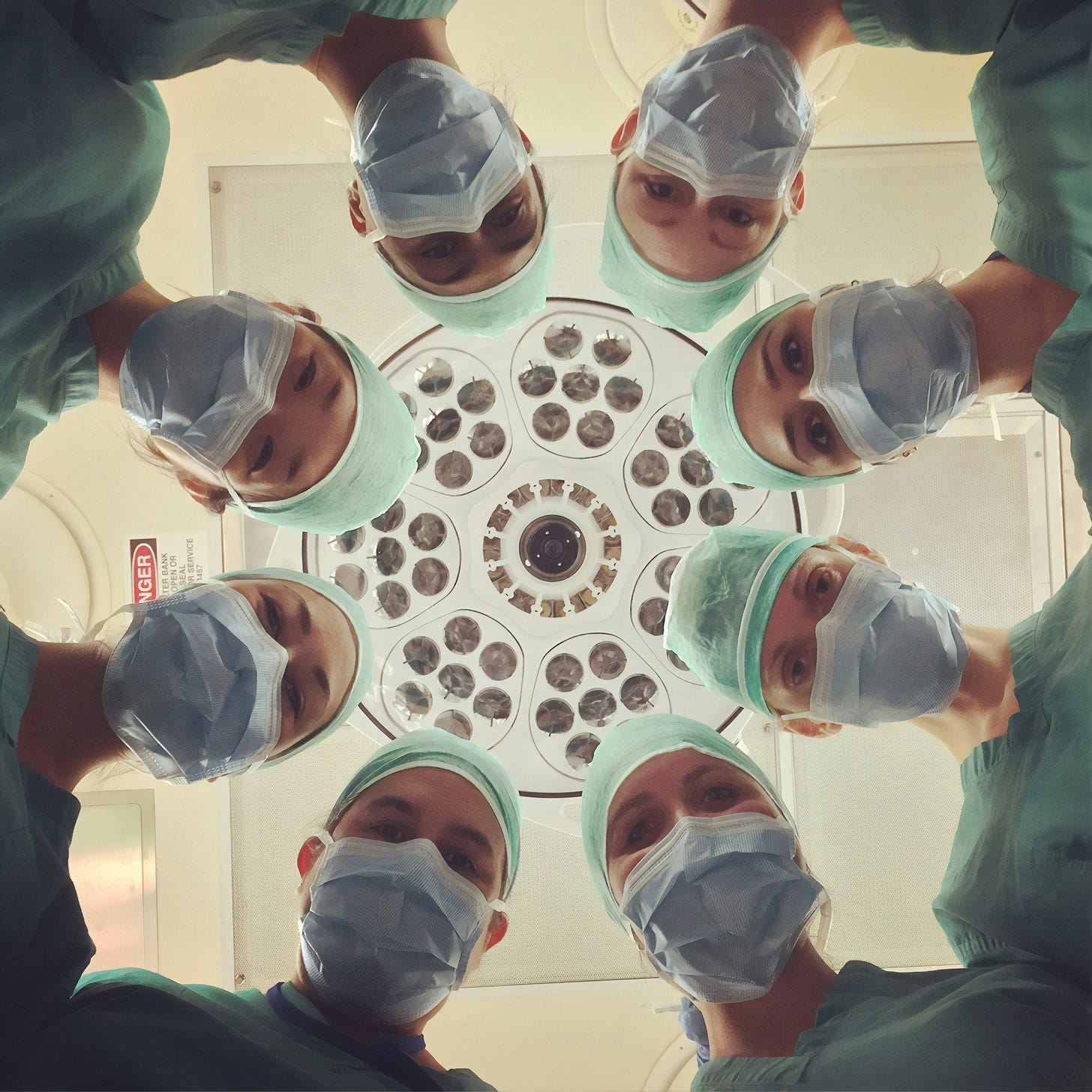
Photo by National Cancer Institute on Unsplash
There is a major disconnect between what older adults want from health care and what the health care system delivers to them.
That disconnect appears on every page of a new study by Age Wave and the John A. Hartford Foundation, titled Meeting the Growing Demand for Age-Friendly Care: Health Care at the Crossroads. When adults aged 65 and older were asked to assign a letter grade to the health care system, only 11% awarded it an A overall. It’s nothing personal – 40% give an A rating to their own health care providers – the problems are systemic.
Take, for example, the health condition that sparks the most fear. For nearly half of older adults, it’s Alzheimer’s or dementia. (Cancer is a distant second at 25%, and Stroke and heart attack trail at 13% each.) Yet just 40% of older adults say their provider routinely evaluates their cognitive function. Even among patients ages 80 and older, the number rises only to 47%.
To Cure or To Care
What the report makes clear is our so-called health care system (which in fact is a patchwork, jerry-rigged mishmash of private providers, state and federal governments, insurers and pharmaceutical companies) is set up in such a way that physicians have no incentive, and little training, to address what concerns older adults most.
The medical system rewards physicians who specialize. It offers few incentives for generalists who can look at the patient as a whole body or, dare we say it, a whole person. It rewards health care workers who treat diseases, especially chronic conditions. But what concerns older adults most is functional – being able to do the activities they enjoy. When asked what they see as the benefits of a long life, three-fourths of older adults answered, “enjoying more time with family and friends” and “continuing to do the activities I love.”
Perhaps physicians would better understand patients’ needs and desires if they had more time to spend with them. But the current system makes that a rare luxury. Doctors are under intense pressure to be efficient in an effort to contain medical expenses.
The complexity of the system is an issue for older patients. It’s no surprise that 56% agreed that “it is difficult and stressful to navigate the health care system,” while 62% said insurance plans offer too many options. More than one-third said dealing with the health care system “has become my part-time job.”
Pervasive Ageism
Louise Aronson, a geriatrician and author of the book Elderhood, blames much of the disconnect on ageism, the pernicious attitude that identifies “old” as “other.” She sees it in medical Education, where “education on care of older adults is too often negligible to very limited and distorted by prejudice.” This is despite the fact that older adults account for about 40% of hospital stays and up to one-third of outpatient visits. “Usually, medical education and health systems are responsive to demographics and epidemiology,” she writes, “but that’s not so when it comes to the needs of older patients.”
Ageism is also to blame, she says, for the fact that older adults were not included in drug trials for new medications. The National Institutes of Health recommended including women and minorities in research trials in 1986, added children in the 1990s, but didn’t recommend including older adults until 2019. As a result, older adults are prescribed medications whose effects on older patients have not been tested.
(For a simple yet comprehensive look at ageism in health care, check out this infographic.)
The health care system needs to offer more age-friendly care, says the Age Wave-Hartford Foundation report. It suggests that physicians should explore with their older patients what it calls the “4Ms Framework:” Medications, Mind, Mobility, and what Matters. One effort to promote such care is the Age-Friendly Collaborative, an effort to accelerate and spread the adoption of evidence-based, age-friendly care. Currently 5,000 care settings have been certified as age-friendly.
As Aronson observes, health care doesn’t have to be this way. Given the sheer number of older adults in the health care system today and the even greater numbers coming in the next three decades, we have the power to change the system by insisting on better, more age-appropriate treatment.