“I’m Worried About Alzheimer’s. Should I Undergo Biomarker Testing?”
In September 2024, over 14,000 eager scientists, researchers, and observers attended the Five-day Alzheimer’s Association International Conference (AAIC). The purpose of this annual assembly is to showcase the most recent advances in Alzheimer’s disease (AD) and dementia.
A “Key Takeaway” From AAIC: New Blood Biomarkers Offer Earliest Diagnosis


The new tests were embraced as “a simple and accurate selection tool for identifying cognitively unimpaired patients who likely have amyloid-beta plaques in their brains”, and as a means to“improve early diagnosis and speed access to treatment.” The blood tests “assess phosphorylated tau (p-tau) protein, an Alzheimer’s biomarker that can build up before patients show signs of cognitive impairment. . . .Increases in the specific marker over time correlate with worsening cognition and brain atrophy. . . .The p-tau217 test also predicts the likelihood of amyloid plaques in the brain, another biomarker for Alzheimer’s and the target of recently approved treatments.”
Simply put, the reliable presence of a unique AD marker in blood, brain, or cerebrospinal fluid is a 100% accurate test for the presence of AD.
Such tests are undeniably “great news for the future of Alzheimer’s research.” Identifying asymptomatic individuals highly likely to develop AD allows investigators to study that population, from their genetics to Lifestyle factors to their responses to behavioral and pharmacologic interventions. The goal being to delay or even prevent the development of Alzheimer’s disease. Such biologically defined AD patients will be essential for all manner of studies and have an easier time qualifying for current anti-amyloid therapies. Highly accurate blood tests for AD will find their way into many more physician practices.
Fast-forward to the likely responses of the pharmaceutical industry and the manufacturers and marketers of such groundbreaking tests when millions of asymptomatic individuals are added to the 8.5 million Americans currently estimated be diagnosed with Alzheimer’s disease by 2030.
BUT… What About Us?
What is best for those of us who are largely asymptomatic, still untested, and potentially blood-test-positive? We’re currently genuinely worried, maybe a somewhat less sharp, have a normal 7-minute office neurological exam (and are still able to draw that stupid clock), a touch absentminded, can’t help thinking about Uncle Leo’s incident with the neighbor lady, and maybe a little slow in remembering names or where we left our glasses . . .
Individual primary care providers may choose to add blood AD biomarkers to our evaluations. Most doctors love testing: they don’t want to miss a diagnosis. Unfortunately, some may fail to adequately consider their patient’s likely response to a positive test. Biomarker testing is not just “another trip to the lab.” Before signing on for one of these exams, ask yourself this question: “How would a positive result change my life?”
The 2024 consensus report, Revised Criteria for Diagnosis and Staging of Alzheimer’s Disease, narrowed the standard for AD diagnosis by declaring biomarker tests as the sole criterion for the diagnosis of Alzheimer’s disease. However, the authors also added:
“First, the clinical use of AD biomarkers is presently intended for the evaluation of symptomatic individuals, not cognitively unimpaired individuals. We highlight the distinction between canand should. AD can be diagnosed in asymptomatic individuals, but we do not believe this should be done for clinical purposes at this time.”[Emphasis added.]
To be clear, I am not talking about genetic testing for the rare early onset autosomal dominant form of Alzheimer’s disease. These account for only 1–5% of all AD patients, but half of the cases that occur before age sixty. An affected child typically has an affected parent. Testing for those whose parents or grandparents developed Alzheimer’s before age sixty-five can reveal one’s risk of carrying the gene and passing it on to their children.
———-
The following personal opinions are based on my 3-year literature review and well over 300 scientific references. They are not medical advice. Talk to your doctor. Feel free to keep my comments in mind (and the recent references found in Aging or Alzheimer’s in hand).
Now That We Know We Can Know – Should We Know?
A diagnosis before the onset of cognitive impairment would drastically alter the lives of millions of patients and their families. Outside of a research setting, few authors have recommended biomarker testing in relatively asymptomatic elderly individuals.
Nearly 75% of those labeled with preclinical Alzheimer’s disease by testing will not progress to clinically evident AD in their lifetimes!
—–
Nor can one predict, for any individual, the time lapse between identifying an early stage of Alzheimer’s and the actual onset of dementia.
Knowing this, one must wonder how carrying such terrible uncertainty—possibly for decades—could affect both one’s self-perception and how others might view them. Such news would certainly create Anxiety for family members about their own potential status as patient or future long-term caregiver.
Finally, since there is still no disease-modifying Therapy for AD, what is the point of knowing? There is no cure. Both the long-available traditional agents for AD and the new anti-amyloid infusions offer, at best, the chance of “turning back the clock on memory loss” for around six months! Even when the “latest and greatest” agents significantly reduced or eliminated brain amyloid levels, patients still got worse. In the absence of effective therapies, many will see no advantage to identifying preclinical AD patients for intervention.
In my reading, I learned that not every experienced neurologist or neuroscientist is enthusiastic about diagnosing preclinical AD in their patients (or themselves): One Mayo Clinic neurologist candidly told a New York Times reporter: “Not everyone does progress. Even when they do, it can be years before there are symptoms. Outside of research studies, we do not do [definitive and diagnostic] amyloid scans on clinically normal people because we don’t know what to tell them [emphasis added].” Another asymptomatic neuroscientist had a negative screening scan as a volunteer subject in a research study. He later admitted that, had the scan been positive, it would have changed his life forever: “I will wake up every morning and wonder whether . . . this is the day I am going to forget something.”
Practical Considerations: Biomarker Testing in Asymptomatic Individuals
Insurance: While health insurers are prohibited by law from denying coverage for Alzheimer’s disease, there is nothing to prevent those writing long-term care policies and life insurance from refusing to enroll someone positive for an AD biomarker.
Health equity is a very real concern. Potentially beneficial supports and interventions are not available to all.
Quality of life: Persons aware of their diagnostic label and its prognosis report a lower quality of life than those unaware of these facts about themselves. The associated sense of loss is unrelated to the actual degree of cognitive impairment.
Why Get Tested?
These tests, if supported by further research, will be able to replace scanning and invasive spinal fluid tests. The new blood tests will do a better job of accurately detecting Alzheimer’s than previous traditional diagnostic methods. With their high negative predictive value, a negative test can definitively exclude AD. In ruling out AD, biomarker testing can stimulate the search for other less common causes of cognitive impairment that are not yet evident clinically. The last thing you want to do is to make decisions based on a false positive diagnosis of AD, leaving potentially treatable etiologies on the table.
“I just have to know.” Family history worries relatives, particularly if there are concerns about early onset AD. And some of us just have to know.
For the greater good: These tests will be invaluable for research. Accurate early diagnoses will allow the study of Alzheimer’s disease in the preclinical stage, potentially leading to better outcomes or even prevention of clinical disease. For those who want to explore every option, there will be no shortage of clinical trials assessing new therapies. Many of these will require biomarker testing as a condition of enrollment. The earlier the diagnosis, the better the chances for access to trials.
My Cautionary Bottom Line:
This is brand new. Take a breath and think it over. Given the absence of preventive means or a cure, there is time to get good advice. Consider the pros and cons as they apply to you and your family.
[No current cure = No rush]
There is always “breaking news” surrounding this widespread and terrible disease. Remember Aducanumab, the first anti-amyloid treatment, approved and withdrawn in 2 ½ years, “a cautionary tale of overpromising, under-delivering, and an inside look at FDA sausage-making” (https://healthjournalism.org/blog/2024/02/adieu-aduhelm-biogen-pulls-plug-on-controversial-alzheimers-drug/#:~:text=On%20Jan.,look%20at%20FDA%20sausage%2Dmaking.)
“It has been a Wild West for AD blood tests,” said Suzanne Schindler, Washington University, St. Louis. “That has brought significant risk. . . . “If clinicians start using these tests and some perform poorly, this can diminish trust in all these biomarkers.” At AAIC, Schindler argued that performance standards are necessary to help ensure accurate and timely diagnosis of Alzheimer’s disease as these tests leave the confines of AD research clinics and start to enter routine clinical care. (https://www.alzforum.org/news/conference-coverage/setting-standards-experts-aim-tame-wild-west-ad-blood-tests)
References (publicly available)
Jack CR Jr, et al. Revised criteria for diagnosis and staging of Alzheimer’s disease: Alzheimer’s Association Workgroup. Alzheimers Dement. 2024 Jun 27. doi: 10.1002/alz.13859. Epub ahead of print. PMID: 38934362. https://alz-journals.onlinelibrary.wiley.com/doi/10.1002/alz.13859),
National Academies of Sciences, Engineering, and Medicine; Division of Behavioral and Social Sciences and Education; Board on Behavioral, Cognitive, and Sensory Sciences. Implications for Behavioral and Social Research of Preclinical Markers of Alzheimer’s Disease and Related Dementias: Proceedings of a Workshop—in Brief. Forstag EH, editor. Washington (DC): National Academies Press (US); 2021 Aug 24. PMID: 34460185. https://nap.nationalacademies.org/catalog/26295/implications-for-behavioral-and-social-research-of-preclinical-markers-of-alzheimers-disease-and-related-dementias
Schindler SE, et al. Acceptable performance of blood biomarker tests of amyloid pathology – recommendations from the Global CEO Initiative on Alzheimer’s Disease. Nat Rev Neurol. 2024 Jul;20(7):426-439. doi: 10.1038/s41582-024-00977-5. Epub 2024 Jun 12. PMID: 38866966. https://www.nature.com/articles/s41582-024-00977-5
and excerpted from:

Originally Published on https://agingoralzheimers.com/
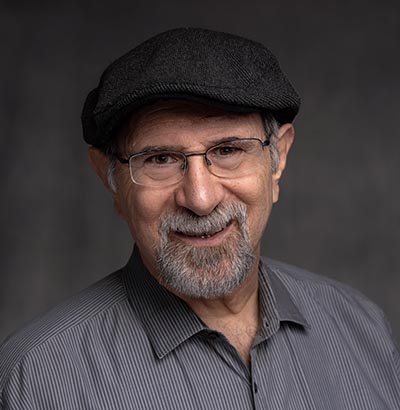
Kenneth Frumkin, PhD, MD, FACEP studied physiological psychology (the interaction of the body’s basic biologic mechanisms with behavior) in college and graduate school. He earned his Masters and Ph.D. degrees from McGill University for his work on the relative contributions of nature and nurture to the ingrained survival mechanism of poison-avoidance in rats. After two years of research at the U.S. Army’s Biomedical Laboratories, Ken went on to medical school and a residency in emergency medicine. His 36-year medical career was split between community hospital emergency departments and teaching, research, and practice in military academic medical centers.
Board-certified in his specialty, Dr. Frumkin is the author of over three dozen peer-reviewed publications and textbook chapters in psychology and medicine. His article “How to Survive the Emergency Room” published in the AARP Bulletin, was a 2022 National Mature Media Merit Award winner. A complete list of publications and complete resume are at www.linkedin.com/in/KennethFrumkinPhDMD . A Fellow and Life Member of the American College of Emergency Physicians and their Geriatric Emergency Medicine Section, Dr. Frumkin is also an Emeritus member of the Society for Academic Emergency Medicine and their Academy of Geriatric Emergency Medicine. Having retired as a civilian employee of the Department of the Navy in 2017, Dr. Frumkin is currently a volunteer member of the academic faculty at the Emergency Medicine Residency, Naval Medical Center, Portsmouth, Virginia.
Dr. Frumkin writes from the perspective of a practiced author and researcher and, most importantly, as a fellow boomer with “skin in the game.” He, too, is seeking the answers to nearly every older-person’s questions about their fluctuating memories and the possibility of progressive cognitive decline. His book "Aging or Alzheimer’s? A Doctor’s Personal Guide to Memory Loss, Cognitive Decline, and Dementia" comes out November 5, 2024. (AgingOrAlzheimers.com)